Osteoarthritis(arthrosis) is a joint disease characterized by degenerative changes in the cartilage that covers the bone, in other words, from its destruction.
%20and%20normal%20cartilage%20(right).jpg)
The vast majority of affected joints are the knee, hip, shoulder, and first metatarsophalangeal. Damage to other joints is much less common and is often secondary. In recent years, the disability caused by osteoarthritis has doubled.
Like any disease, osteoarthritis also has risk factors for its development, which are actively studied today, and the list is expanding every year. The main ones are considered:
- age;
- inheritance;
- metabolic disorders;
- weight gain;
- osteoporosis;
- inadequate and irregular nutrition;
- endocrine disorders;
- menopause;
- frequent hypothermia;
- trauma;
- arthritis (inflammation of the joint);
- foci of chronic infection or inflammation (for example, chronic tonsillitis).
- Varicose veins.
If you find similar symptoms, consult your doctor. Do not self-medicate - it is dangerous for your health!
Symptoms of Osteoarthritis
Common symptoms of osteoarthritis include:
- pain during exertion;
- limitation of movement in the joint;
- feeling of stiffness in the morning, feeling of "crunch";
- pain after a long rest (the so-called "starting").
Joint pain is rarely sharp, more often aching or dull, and usually stops during rest. Symptoms are often undulating and can come and go without trying to treat. They can be mild, moderate or severe. Complaints in osteoarthritis may remain roughly the same for many years, but over time they progress and the condition worsens. Minor and moderate symptoms can be controlled at the same level, but the severe course of the disease can lead to chronic pain, inability to carry out daily household activities, leading to disability, up to and including disability.
Pathogenesis of arthrosis
The main nutrient for the joint isthe synovial fluid. It also plays the role of a lubricating agent between the joint surfaces. A huge and important role in the development of osteoarthritis is assigned to metabolic processes in the joint and its structures. At the initial stage, when biochemical disorders develop in the synovial fluid, its properties decrease, triggering the mechanism of destruction. The first to hit is the synovial membrane of the joint, which plays an important role as a membrane and is a kind of filter for the most important nutrient of the cartilage - hyaluronic acid, preventing it from leaving its main workplace - the cavity. articulate. The saturation of the properties of the joint fluid determines its circulation, which cannot ignore the regular movement of the joint itself. Hence the famous phrase "movement is life". The constant circulation of synovial fluid in the joint cavity is the key to a complete metabolism in it. With a lack of nutrients, the cartilage becomes thinner, the formation of new cells stops, the joint surface becomes uneven, rough, with areas of defects. The relationship between diseases of the veins of the lower limbs (for example, varicose veins) and lo is knowndevelopment of metabolic disorders in the joints, mainly of the knee. The bone structure under the cartilage responds to the process with a compensatory mechanism: it thickens, becomes coarser and expands the coverage area, resulting in the formation of exostoses and osteophytes, which is the main reason for the limitations and deformities of the joint. The synovial fluid is saturated with inflammatory cells and decay elements, the joint capsule in response to this thickens, becomes rough and loses elasticity, the soft tissues literally become dry (dehydration occurs), hence the disturbances of morning stiffness, " initial pains ". The pathological process in the last stages causes the body to activate the last compensatory mechanism: immobilization. At rest and in the so-called physiological position, pain is minimal, the ligament apparatus is maximally straightened. In this position, the joint tends to become fixed, and succeeds in the rapid formation of coarser exostoses, which "fix" the joint, and the patient loses the ability to move it completely. The muscles of such a limb are hypotrophied, become weaker and smaller. Such changes are already considered irreversible.
Classification and stages of development of osteoarthritis
The disease is divided into 2 large groups: primary (or idiopathic) and secondary. The first group develops due to an unclear reason or as a result of age-related changes. The second is characterized by clear causes and develops due to their pathological process (for example, against the background of tuberculosis, osteochondritis dissecans, subchondral necrosis, etc. )
Regardless of the reasons that contributed to the development of osteoarthritis, there are 4 stages of its development:
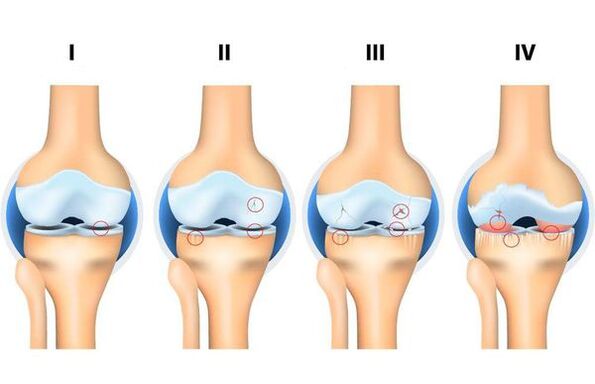
- Stage 1: the hard structures of the joint are not involved in the process of destruction, there are initial changes in its soft structures and in the composition of the joint fluid (which is a nutrient medium and reduces friction of the joint), there is a malnutrition of the joint.
- Phase 2: accompanied by the "beginning" of the mechanism of destruction of the solid structures of the joint, solid border formations (exostosis, osteophytes) are formed. Moderate complaints of changes in range of motion.
- Stage 3: accompanied by a narrowing of the joint lumen, pronounced destruction of the loaded surface with the formation of osteochondral defects, pronounced limitation of movement, a constant feeling of "crunch" during movement, initial changes in the axis of the limb.
- Stage 4 - severe, in which movements are clearly limited in the joint up to its complete absence (ankylosis), a pronounced inflammatory process, its deformation, the formation of bone defects (as a result of the complete absence of cartilage cover).
Complications of osteoarthritis
Without treatment, any disease causes complications, and osteoarthritis is no exception. If this is the primary form, the main complications include:
- damage to the soft structures of the joint (degenerative tears of the menisci, ruptures of the ligaments, etc. );
- chronic inflammatory process;
- ankylosis (complete absence of movement in the joint);
- deformation of the joint.
If this is a secondary form, the complications depend on the process that caused the development of arthrosis. For example, it can lead to osteoporosis, a chronic disease characterized by a progressive disorder of bone metabolism. As a result, the bones become fragile, their nutrition is disturbed, as a result, osteoarthritis is complicated by the threat of intra-articular fractures. Therefore, it is so important to see a doctor in a timely manner. As the eminent surgeon wrote: "The future belongs to preventive medicine".
Osteoarthritis Diagnosis
Diagnosis of osteoarthritis often begins with a doctor (usually an orthopedic traumatologist) from the first-line medical care (polyclinic), where a clinical examination is performed and the examination data (CT, MRI, X-rays, etc. ) are interpreted to determine the degree and type of osteoarthritis. . . Diagnosis and diagnosis are usually straightforward. If the diagnosis is unclear or the doctor suggests a secondary development of the disease, the patient is referred to doctors of other specialties (for example, a rheumatologist) for clarification. It is very difficult to determine the degree of osteoarthritis without examination results. The history of the disease, methods and attempts of treatment are also important for the diagnosis and determination of treatment tactics, as the doctor often faces the difficult task of differential diagnosis (for example, the symptoms of osteoarthritis and arthritis often coincide).
Treatment of osteoarthritis
Over the initial stages of osteoarthritis amenable to conservative treatment, they provided an integrated approach. The treatment takes a long time and has the main objective: to stop the destruction process at the stage in which the treatment was started or to slow down this process. The complex includes pharmacological and non-pharmacological treatment, which includes courses in physical therapy (physiotherapy and gymnastics exercises), physiotherapy (usually phonophoresis and magnetotherapy), swimming, anti-inflammatory therapy (ingestion or topical in the form of gel or cream), chondroprotective therapy (taking drugs based on cartilaginous components) and intra-articular injections (these can be both homeopathic medicines and hyaluronic acid preparations). Chondroprotectors are still used by orthopedic traumatologists, they are prescribed by internal courses, but the results of recent scientific studies in Western countries refute the positive effect compared to the placebo effect. With severe symptoms and severe stages, conservative treatment becomes ineffective, which puts surgical treatment first. Given the indications, it can be both a minimally invasive treatment - arthroscopy and endoprosthesis. With arthroscopy (endoscopy of the joint), it is disinfected under the control of video optics, exostoses are removed (if possible) and damage to soft structures, which is often observed in such stages, is removed. Recently, however, the benefits of this type of surgery for osteoarthritis have been increasingly questioned, as it does not have the desired effect in chronic pain, and in some cases it can cause significant damage if performed poorly.
Endoprosthesis is a technically difficult and difficult operation, the purpose of which is to create a completely new artificial joint. It requires clear indications and identification of risks in the presence of contraindications. Endoprostheses for the knee, hip and shoulder joints are being used successfully today. Additional outpatient supervision by a doctor reduces the risks and terms of rehabilitation, improves the quality and efficiency of the operation performed.
Forecast. Prophylaxis
The forecast depends on a timely visit to an orthopedic-traumatologist and the onset of a treatment complex. In terms of eliminating morphological changes in osteoarthritis, the prognosis is unfavorable, since it is impossible to completely restore the cartilage structure of the joint. In old age, the course of the disease is more severe than in young people. However, with timely access to a doctor and compliance with all recommendations, it is possible to eliminate all complaints and restore full motor function of the joint.
Preventive measures:
- Regular physical activity.It is a misconception that physical activity can "wear out" a joint. Augmented - yes, but not regular and moderate. According to the latest data, any activity aimed at strengthening and maintaining muscle mass, by improving coordination, supports the motor function of the joints and their blood supply. Any physical activity allows you to achieve regular circulation of joint fluid, which is the main source of nutrition for the joint and its structures. People who use public transport every day and have foot traffic are known to be less likely to develop osteoarthritis.
- Body weight control and its adequate reduction.The increase in mass increases the load on the joints of the lower extremities and the spine. Therefore, any protocol for the rehabilitation and conservative treatment of osteoarthritis includes a course of LFT (physiotherapy and gymnastics exercises).
- Correction and elimination of congenital deformities.An important role is played by flat feet, which over the years lead to a violation of the axis of the legs, which entails a disproportionate increase in the load on certain parts of the joints and spine, deforming them.
- Proper nutrition.It allows you to create conditions for full enrichment of the joint with nutrients. Therefore, the refusal of a large number of foods, frequent diets, irregular feeding of low-substance foods (fast food, etc. ) can become a "trigger" for the development of osteoarthritis.
- Timely elimination of concomitant diseases.The now forgotten medical tests made it possible to identify and eliminate diseases in an early stage. Concomitant diseases can be a significant cause of the development and progression of osteoarthritis (for example, diseases of the endocrine system, gastrointestinal tract, chronic foci of infection or inflammation).




















